Migraine is a common and often misunderstood condition, especially when it comes to hormonal changes and migraines in women. Although both men and women suffer from migraines, they’re known to be more prevalent among women due largely in part to their connection to female hormones.1
Understanding Female Hormones
Think of hormones like the body’s messengers that travel through your bloodstream, telling your organs and systems what to do. Two of the hormones that play a major role for women are:
- Estrogen: In addition to regulating the menstrual cycle, estrogen also affects the reproductive and urinary tract, bone density, breasts, mood, skin, and hair, among other functions.2
- Progesterone: This hormone steps in during the second half of a menstrual cycle. Its job is to prepare the uterus for pregnancy and maintain a fertilized egg. Progesterone levels rise after ovulation.
The Role of Hormones in Menstrual Migraines
Many women experience a migraine just before or during their menstrual cycle. In fact, more than half of women who struggle with migraine notice a link with their periods, according to the National Migraine Center.
A menstrual migraine, also known as a hormonal migraine, is often longer and more severe than migraine attacks at other times of the month,3 and it’s most likely to occur either two days before a period or the first three days of the period.
Estrogen and progesterone levels rise and fall at different times during the menstrual cycle—this rollercoaster ride impacts the blood vessels in the brain, which can sometimes trigger a migraine, especially for women already prone to them. Some women who take an oral contraceptive pill report more frequent migraine attacks, especially during the pill-free week when estrogen levels drop.
Perimenopause, Menopause, and Migraine
Perimenopause refers to the months and years leading up to menopause. Estrogen and progesterone levels continue to rise and fall in the perimenopause stage. As women get closer to the menopause stage, menstrual cycles get shorter, and estrogen levels decline more rapidly, which is believed to be what leads to migraine attacks at this stage of life.
Studies have shown that women in the perimenopause stage have a greater risk of developing high-frequency migraines (10 or more migraines a month) than premenopausal women.4 Many women also start experiencing migraines for the first time during perimenopause.5
The good news is that estrogen levels usually stabilize in the menopause stage, which for many women means the end to their hormone-related migraines.
Managing Hormonal Migraines
If you suspect you may be getting menstrual migraines, try keeping a diary for at least three cycles, which will help you determine if there is, in fact, a connection. The diary will also help you pinpoint at what stage in your cycle you get a migraine (before or at the start of a period).
There are several things you can try for managing hormonal headaches, including hormonal birth control to stabilize estrogen levels or migraine medications. However, these methods may not be effective for all women and can pose risks if you are pregnant or trying to conceive. Other tips for managing menstrual migraine include:
- Eating small, frequent snacks to maintain your blood sugar level.
- Maintaining a regular, consistent sleep pattern.
- Finding ways to manage stress.
Fortunately, there’s a non-drug solution to treat menstrual migraine that is safe for women who are 12 and older. gammaCore™ non-invasive vagus nerve stimulator (nVNS) is a handheld device that treats and prevents migraine when used twice daily. It’s available with a prescription and is easy to use at home or on the go—each treatment session takes less than five minutes. It can also be used up to 24 times daily for fast-acting migraine relief when needed.
Why Choose gammaCore nVNS to Manage Your Menstrual Migraine?
gammaCore is designed to be used when migraines affect women most and without the use of additional medications.6 Here are a few reasons to consider adding gammaCore to your menstrual migraine relief toolkit:
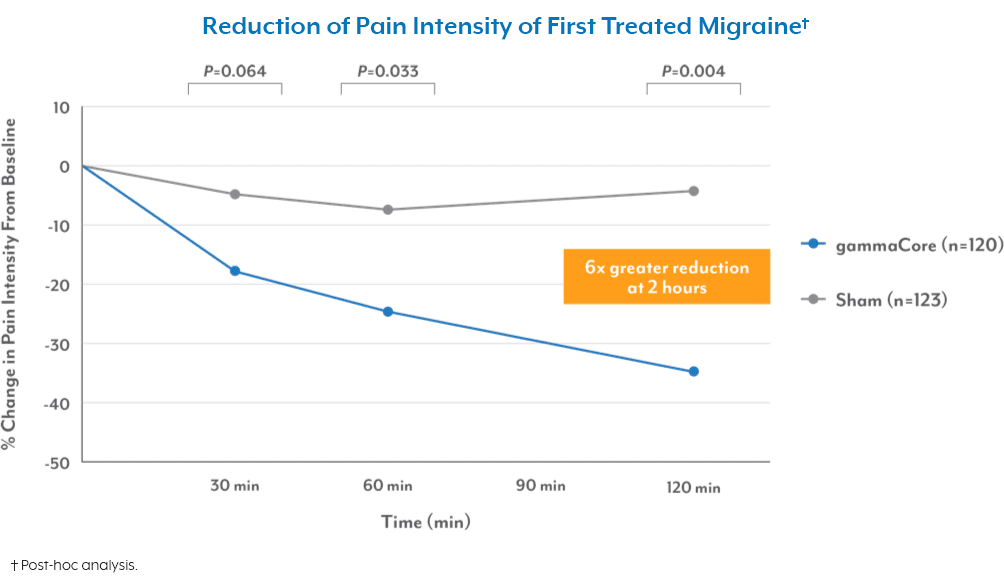
- It works fast. It can provide fast relief from the first treated attack in as little as 30 minutes after treatment, and without any pills or drug-related side effects.7
- It’s safe to use. gammaCore is clinically tested to be safe and tolerable.8
- It delivers results. One open-label study found that gammaCore reduced the average number of menstrual migraine and menstrual-related migraine days by 35%, with nearly 40% of patients experiencing a reduction of more than 50%. gammaCore also reduced the intensity of the migraines that did occur and reduced the use of pain medication to acutely treat the migraine attacks by 37%.9
To see if gammaCore is right for you, visit our clinic finder to locate a health care provider near you, or contact our dedicated Customer Experience team at 888-903-2673 or customerservice@electrocore.com.
References
1. Walter, K. (2022). What Is Migraine? Journal of the American Medical Association, 327(1).
https://doi.org/10.1001/jama.2021.21857
2. Estrogen’s Effects on the Female Body. Johns Hopkins Medicine. Retrieved September 7, 2023, from https://www.hopkinsmedicine.org/health/conditions-and-diseases/estrogens-effects-on-the-female-body
3. (2021, November 5). Menstrual Migraine Treatment and Prevention. American Migraine Foundation. Retrieved September 7, 2023, from https://americanmigrainefoundation.org/resource-library/menstrual-migraine-treatment-and-prevention/
4. Martin, V. T., Pavlovic, J., Fanning, K. M., Buse, D. C., Reed, M. L., & Lipton, R. B. (2016). Perimenopause and Menopause Are Associated With High Frequency Headache in Women With Migraine: Results of the American Migraine Prevalence and Prevention Study. Headache, 56(2), 292-305. https://doi.org/10.1111/head.12763
5. Doherty, C. (2023, July 13). Perimenopause and Migraines. Verywell Health. Retrieved September 7, 2023, from
6. Grazzi, L., Egeo, G., Calhoun, A. H., McClure, C. K., Liebler, E., & Barbanti, P. (2016). Non-invasive Vagus Nerve Stimulation (nVNS) as mini-prophylaxis for menstrual/menstrually related migraine: an open-label study. Journal of Headache and Pain, 17(1). https://doi.org/10.1186/s10194-016-0684-z
7. Tassorelli, C., Grazzi, L., De Tommaso, M., Pierangeli, G., Martelletti, P., Rainero, I., Dorlas, S., Geppetti, P., Ambrosini, A., Sarchielli, P., Liebler, E., & Barbanti, P. (2018c). Noninvasive vagus nerve stimulation as acute therapy for migraine: The randomized PRESTO study. Neurology, 91(4), e364–e373. https://doi.org/10.1212/wnl.0000000000005857
8. Ben-Menachem, E., Revesz, D., Simon, B. J., & Silberstein, S. D. (2015). Surgically implanted and non‐invasive vagus nerve stimulation: a review of efficacy, safety and tolerability. European Journal of Neurology, 22(9), 1260–1268. https://doi.org/10.1111/ene.12629
9. Grazzi, L., Egeo, G., Calhoun, A. H., McClure, C. K., Liebler, E., & Barbanti, P. (2016). Non-invasive Vagus Nerve Stimulation (nVNS) as mini-prophylaxis for menstrual/menstrually related migraine: An open-label study. The Journal of Headache and Pain, 17(91). https://doi.org/10.1186/s10194-016-0684-z