If you’ve ever experienced a throbbing, debilitating headache, you may have been experiencing a migraine. But what is migraine, really? At its core, a migraine is more than just an ordinary headache. It’s a complex neurological condition often described as severe and intense pulsing or throbbing, usually on one side of the head. The pain can be so severe that it’s difficult to focus on anything else. A migraine can last for hours or even days and significantly impact your day-to-day life.
Migraines affect a substantial portion of the global population. Migraines affect 1 in 7 people globally, with over 35 million people in the U.S. suffering from this condition. The impact is widespread, as 1 in every 4 American households has a member who suffers from migraines.
What Causes Migraine?
Migraine pain is believed to be caused by activated nerve fibers1 within the wall of brain blood vessels. Migraine attacks can be triggered by several potential factors, including:
- Changes in Sleep Patterns: Sleeping too much or too little can trigger a migraine. Studies have shown a connection between poor sleep quality and the frequency of migraine.2
- Hormonal Changes: Fluctuations in estrogen levels, such as during the menstrual cycle, can trigger migraine for some women. Many men who suffer from migraines have increased levels of the estradiol hormone (a form of estrogen) and lower levels of male hormones, like testosterone.3
- Stress and Emotional Factors: High stress, anxiety, or even excitement can lead to a migraine episode.
- Environmental Factors: Bright lights, loud noises, strong smells, and changes in weather have been known to trigger migraine in some individuals.3
- Certain Foods and Drinks: Foods that contain the chemical tyramine, like aged cheeses and processed meats, can trigger a migraine. Alcohol and the additive MSG (monosodium glutamate)4 have also been identified as potential migraine triggers.
Types of Migraine
Migraine with Aura
Migraine with aura is a specific type of migraine where individuals experience neurological symptoms before or during the headache phase. These symptoms, known as auras, can include visual disturbances, sensory changes, or speech difficulties. Approximately 25-30% of migraine sufferers experience auras.
Other Types of Migraine
There are several other types of migraine, including:
- Chronic migraine: Headaches occurring on 15 or more days per month for more than three months
- Vestibular migraine: Characterized by vertigo and dizziness
- Hemiplegic migraine: A rare form that can cause temporary paralysis on one side of the body
- Retinal migraine: Affecting vision in one eye
Understanding the specific type of migraine you experience can help determine the most effective treatment approach.
Common Symptoms of a Migraine
Migraine comes with a host of symptoms beyond just severe head pain. The symptoms can vary from person to person and from one episode to another. Some of the most common symptoms include:
- Auras: These are visual disturbances typically experienced before the onset of a migraine. Auras can include flashing lights, zig-zag lines, or blind spots. They usually last anywhere from 10 minutes to an hour.
- Sensitivity to Light and Sound: Even the softest light or sound can feel unbearable during a migraine.
- Nausea and Vomiting: The severe pain can trigger bouts of nausea and vomiting for some migraine sufferers.
- Dizziness: Migraine can leave some feeling disoriented and confused.
- Fatigue and Difficulty Concentrating: Enduring a migraine can leave some feeling weak, drained, and exhausted, which makes it hard to focus on anything else.
Migraine Phases
Prodrome
The prodrome phase, also known as the “pre-headache” phase, can occur hours or days before the actual migraine attack. Symptoms may include mood changes, food cravings, neck stiffness, and increased yawning.
Aura
Not all migraines include an aura phase. For those that do, it typically occurs just before or during the headache phase. Aura symptoms are usually visual but can also affect other senses or speech.
Attack
This is the main phase of the migraine, characterized by an intense headache and associated symptoms like nausea and sensitivity to light and sound. It can last from 4 to 72 hours.
Post-drome
After the headache subsides, many people experience a “migraine hangover” or post-drome phase. This can include feelings of fatigue, confusion, and mood changes that can last for a day or more.
Understanding these phases can help individuals better manage their migraines and potentially identify early warning signs.
Strategies for Relief
Because everyone’s migraine experience is different, there is no “one-size-fits-all” solution. However, there are several strategies that can help alleviate the pain, reduce the frequency of attacks, and prevent migraines from coming on, including tracking your triggers, exercising regularly, eating well and staying hydrated, and prioritizing healthy sleep habits.
You also have the option of preventive medication and treatments. While there are over-the-counter options available, it’s important to consult a health care professional so that they can provide personalized guidance and treatment options.
Treatment Options
Medication
Various medications are available for both acute treatment and prevention of migraines. These include:
- Over-the-counter pain relievers
- Triptans
- CGRP antagonists
- Preventive medications like beta-blockers or antidepressants
Non-Drug Approaches
Non-pharmacological treatments are becoming increasingly popular and can be effective for many individuals. These include:
- Biofeedback
- Cognitive-behavioral therapy
- Acupuncture
- Relaxation techniques
The choice of treatment should be tailored to each individual’s specific needs and migraine patterns.
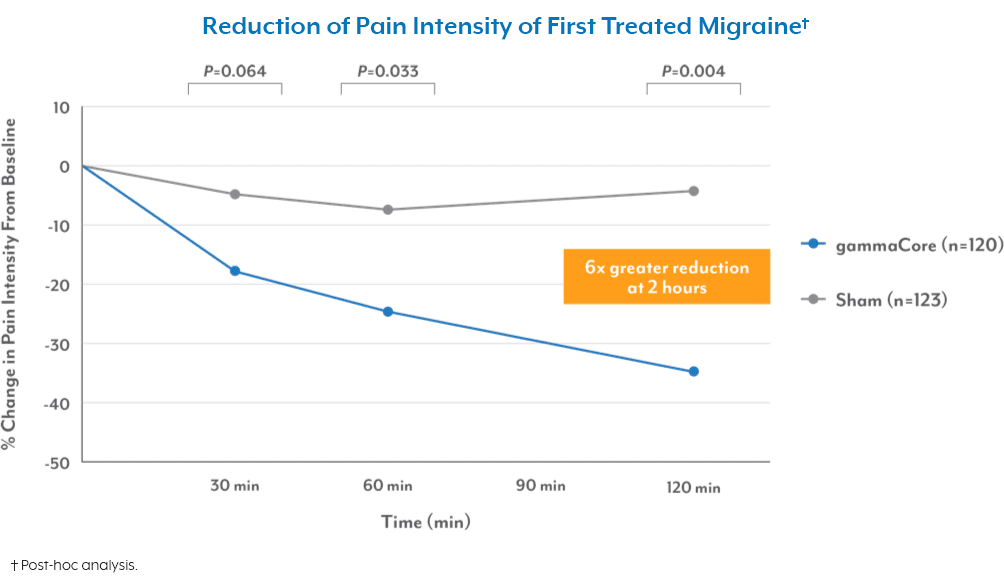
If you suffer from frequent or severe migraines, you may want to speak to your health care provider about innovative, non-drug options, like gammaCore™ non-invasive vagus nerve stimulator (nVNS). Available with a prescription, this portable, FDA-cleared, handheld device works by blocking the pain signals, thereby relieving and preventing migraine pain without the need for surgery or medications. The best part is that you can administer gammaCore nVNS yourself at home or while on the go. Treatment sessions are quick and easy with two 2-minute stimulations, morning and night, on the same side of the neck. You can use it up to 24 times daily for fast-acting relief, when needed.
When to See a Health Care Provider
While occasional migraines can often be managed at home, it’s important to consult a healthcare provider if:
- Your migraine patterns change or worsen
- You experience new or unusual symptoms
- Your migraines interfere significantly with your daily life
- Over-the-counter medications do not provide relief
Only 50% of Americans suffering from migraines had seen a doctor for headache-related reasons in the previous 12 months. Seeking professional help can lead to better management and improved quality of life.
Latest Research and Innovations in Migraine Treatment
The field of migraine treatment is rapidly evolving, with new therapies and technologies emerging. Recent innovations include:
- CGRP monoclonal antibodies for migraine prevention
- Neuromodulation devices like gammaCore
- Advanced neuroimaging techniques for better understanding of migraine mechanisms
The global migraine drugs market is expected to reach a value of $3.72 Billion by 2025, indicating significant investment in research and development of new treatments.
To see if gammaCore is right for you, visit our clinic finder to locate a health care provider near you, or contact our dedicated Customer Experience team at 888-903-2673 or customerservice@electrocore.com.
References
1. Migraine. National Institute of Neurological Disorders and Stroke. Retrieved August 9, 2023, from https://www.ninds.nih.gov/health-information/disorders/migraine
2. Lin, Y. K., Lin, G. Y., Lee, J. T., Lee, M. S., Tsai, C. K., Hsu, Y. W., Lin, Y. Z., Tsai, Y. C., & Yang, F. C. (2016). Associations Between Sleep Quality and Migraine Frequency. Medicine (Baltimore), 95(17). https://doi.org/10.1097/MD.0000000000003554
3. Friedman, D. I., & De ver Dye, T. (2009). Migraine and the Environment. Headache. https://doi.org/https://headachejournal.onlinelibrary.wiley.com/doi/pdf/10.1111/j.1526-4610.2009.01443.x
4. Obayashi, Y., & Nagamura, Y. (2016). Does monosodium glutamate really cause headache? : A systematic review of human studies. The Journal of Headache and Pain, 17(54). https://doi.org/10.1186/s10194-016-0639-4