Everyone is likely to experience a headache at some time or another. However, for those who suffer from paroxysmal hemicrania, it’s a daily struggle that often goes unnoticed by others. Paroxysmal hemicrania is more than just a typical headache. It’s a rare and painful primary headache disorder characterized by intense bursts of stabbing or piercing pain concentrated around or behind the eye on one side of the head. The term “hemicrania” means half-head, indicating the one-sided nature of the attacks.
Paroxysmal hemicrania can be chronic, meaning daily attacks over a year or more, or episodic, where the frequency of attacks can decrease or disappear entirely for months or years at a time.1
Symptoms of Paroxysmal Hemicrania
Individuals with paroxysmal hemicrania will experience sudden and severe attacks that can last anywhere from 2 to 30 minutes, with multiple attacks occurring throughout the day. Some people can experience five attacks throughout day; others may experience as many as 40 attacks in a single day. These attacks can be so intense that they disrupt daily activities, making it challenging for sufferers to maintain a regular routine.
In addition to the pain, sufferers may also experience other symptoms as well, including:
- Red, teary eyes
- Nasal or sinus congestion
- Drooping or swollen eyelid on the affected side
- Facial flushing or swelling on the affected side
- Dull pain or soreness between attacks
Diagnosing Paroxysmal Hemicrania
There is no definitive diagnostic test for paroxysmal hemicrania. Diagnosing the condition involves a thorough examination by a health care professional. A detailed medical history and a description of the symptoms are crucial for an accurate diagnosis. In many cases, a health care provider will recommend imaging tests, such as an MRI, to rule out other underlying causes for the headaches. They may also recommend an MRI if atypical symptoms appear or the individual doesn’t respond to their treatment plan.
Treating Paroxysmal Hemicrania
While there is no known cure, there are several treatment options that can help manage and alleviate the symptoms.
Medications
The first line of defense against paroxysmal hemicrania is usually a non-steroidal anti-inflammatory drug (NSAID) called indomethacin. Many individuals may experience rapid relief when taking indomethacin.2 Responsiveness to this drug is also often used to confirm a paroxysmal hemicrania diagnosis.3 In cases where indomethacin is not well-tolerated or effective, a health care provider may recommend other medications.
Lifestyle Modifications
Stress management, maintaining regular sleep patterns, and avoiding triggers can play a crucial role in managing paroxysmal hemicrania symptoms.
Non-Drug Medical Technology
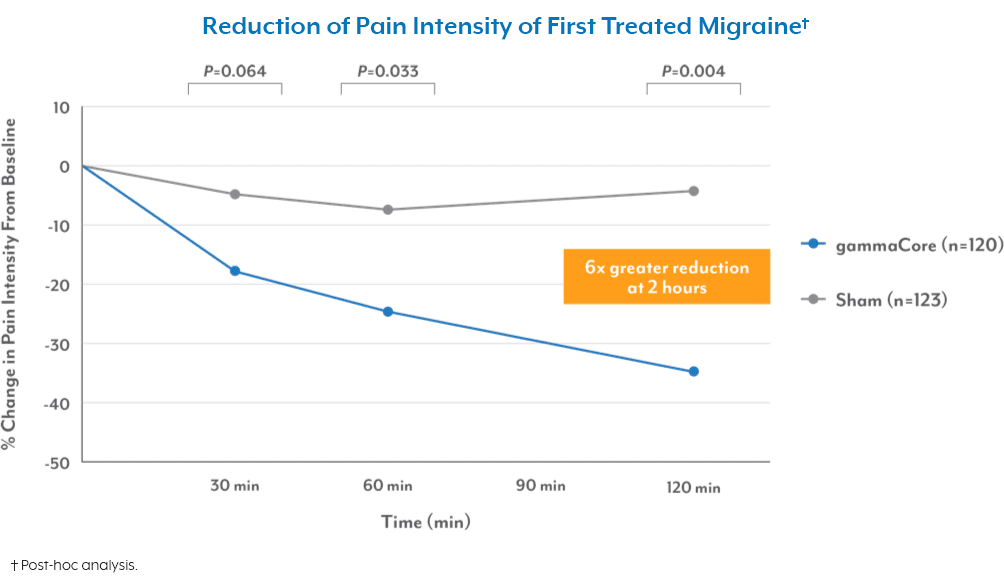
Although indomethacin can provide relief for many, it may not work for everyone, and like any medication, there is always the risk of side effects. The good news is there’s a non-drug option for treating paroxysmal hemicrania. gammaCore™ non-invasive vagus nerve stimulator (nVNS) is a portable, easy-to-use medical device that provides clinically proven relief from multiple types of headache pain.
Several studies have shown non-invasive vagus nerve stimulation to be effective in reducing the severity and frequency of paroxysmal hemicrania headaches, particularly for people who don’t respond to indomethacin or who cannot tolerate the drug.4
The best part about gammaCore nVNS is that it’s available with a prescription, and you can do the treatments yourself at home or on the go. You can use the device to prevent headache pain before it starts and relieve pain when an attack strikes without worrying about drug-related side effects.
To see if gammaCore is right for you, visit our clinic finder to locate a health care provider near you, or contact our dedicated Customer Experience team at 888-903-2673 or customerservice@electrocore.com.
References
1. Paroxysmal Hemicrania. National Institute of Neurological Disorders and Stroke. Retrieved January 9, 2024, from https://www.ninds.nih.gov/health-information/disorders/paroxysmal-hemicrania
2. (2016, May 27). Paroxysmal Hemicrania. American Migraine Foundation. Retrieved January 9, 2024, from https://americanmigrainefoundation.org/resource-library/parosyxmal-hemicrania/
3. (2016, May 27). Paroxysmal Hemicrania. American Migraine Foundation. Retrieved January 9, 2024, from https://americanmigrainefoundation.org/resource-library/parosyxmal-hemicrania/
4. Villar-Martinez, M. D., & Goadsby, P. J. (2023). Non-invasive neuromodulation of the cervical vagus nerve in rare primary headaches. Frontiers in Pain Research. https://doi.org/10.3389/fpain.2023.1062892