Migraines are severe, debilitating experiences that can significantly impact daily life. Interestingly, women are much more likely to suffer from migraines than men. Research shows that women are three times more likely to experience migraines.1 There are a few different factors that can contribute to this stark difference.
Migraines are severe, debilitating experiences that can significantly impact daily life. Interestingly, women are much more likely to suffer from migraines than men. Research shows that women are three times more likely to experience migraines.1 There are a few different factors that can contribute to this stark difference.
Hormonal Fluctuations
One of the primary reasons women are more prone to migraine attacks is hormonal fluctuations. Hormones, particularly estrogen, play a significant role in the frequency and severity of migraines. Estrogen levels fluctuate throughout a woman’s life—during menstrual cycles, pregnancy, and menopause. These changes are known to trigger migraines or worsen existing ones.
Menstrual Migraines: Many women experience migraines around their menstrual period, commonly referred to as menstrual migraine. These typically occur just before or during menstruation when estrogen levels drop sharply.2 It’s estimated that as many as 60-70% of women experience menstrual migraine, according to clinical experience.3
Pregnancy and Migraine: During pregnancy, estrogen levels rise significantly, which can sometimes lead to a reduction in migraine frequency. However, for some women, the hormonal change during pregnancy can trigger migraines, especially in the first trimester.
Menopause: The transition to menopause, known as perimenopause, involves significant hormonal changes that can increase the frequency and intensity of migraines. Post-menopause, some women find relief from migraines as hormone levels stabilize again.
Genetics
Genetics also play a crucial role in migraine among women. Studies have shown that if you have a close family member who suffers from migraines, your chances of experiencing them may be higher.4 While both men and women can inherit these genes, the interaction between genetic predisposition and hormonal factors makes women more susceptible.
There are two types of genetic factors for migraine: association and causal.5 The most common types of migraines are believed to be caused by association, which is the idea that there are a few different genes involved in susceptibility; if you inherit a particular variation of those genes, you’re more likely to suffer from migraines. Other types of migraines are caused by certain genetic mutations; if you inherit those mutations, you’ll inherit a specific type of migraine – in other words, there is a causal relationship here between genetics and migraine.6
Environmental and Lifestyle Factors
Women often juggle multiple roles and responsibilities, which can contribute to stress, a known migraine trigger. Balancing work, family, and social obligations can lead to chronic stress and inadequate sleep, both of which are known triggers that can increase the likelihood of migraines. Additionally, dietary factors, such as skipping meals or consuming certain foods and drinks, can trigger migraines – yet another factor that can lead to migraine risk among women.
Sensitivity to Environmental Triggers
Research has shown that women tend to be more sensitive to environmental triggers such as bright lights7, strong smells8, and loud noises9. As a result, these triggers can set off migraines more easily in women than in men. On top of that, weather changes, high humidity, and even changes in barometric pressure can lead to migraine attacks.
Understanding and Managing Migraine in Women
Understanding the unique factors that contribute to migraine in women is essential for effective management. Here are some strategies that can help:
- Tracking Triggers: Keeping a migraine diary to track triggers can be helpful. Noting down food intake, sleep patterns, stress levels, menstrual cycles, and other hormonal changes can help identify and avoid specific triggers.
- Healthy Lifestyle Choices: Maintaining a regular sleep schedule, managing stress through relaxation techniques, and eating a balanced diet can reduce the frequency of migraines.
- Medical Treatments: Various medications are available to help manage migraines. Consulting a health care professional to find the right treatment plan is crucial.
An Innovative Approach to Help Women Manage Their Migraine
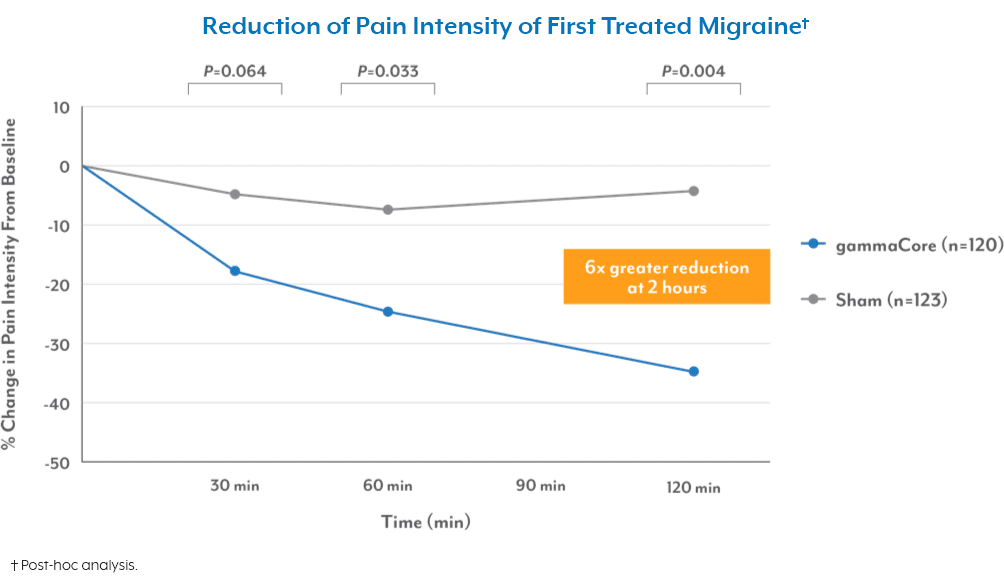
For those seeking an alternative to traditional medications, there is another innovative option that treats and prevents migraine without pills, injections, or drug-like side effects. gammaCore™ non-invasive vagus nerve stimulator (nVNS) provides relief by stimulating the nerve that plays a role in regulating pain. gammaCore nVNS is a portable, handheld device that’s easy to use at home. Use it twice daily for migraine prevention or as needed for pain relief.
To see if gammaCore is right for you, visit our clinic finder to locate a health care provider near you, or contact our dedicated Customer Experience team at 888-903-2673 or customerservice@electrocore.com.
References
1. Rossi, M. F., Tumminello, A., et al. (2022). Sex and gender differences in migraines: A narrative review. Neurological Sciences, 43(9), 5729–5734. https://doi.org/10.1007/s10072-022-06178-6
2. Moy, G., & Gupta, V. (2024). Menstrual-Related Headache. StatPearls Publishing LLC.
3. Silberstein, S. D. (1999). Menstrual migraine. Journal of Women’s Health & Gender-Based Medicine, 8(7), 919-31. https://doi.org/10.1089/jwh.1.1999.8.919
4. Bron, C., Sutherland, H. G., & Griffiths, L. R. (2021). Exploring the Hereditary Nature of Migraine. Neuropsychiatric Disease and Treatment, 17, 1183–1194. https://doi.org/10.2147/NDT.S282562
5. (n.d.). Genetics and migraine. The Migraine Trust. Retrieved August 13, 2024, from https://migrainetrust.org/understand-migraine/genetics-and-migraine/
6. (n.d.). Genetics and migraine. The Migraine Trust. Retrieved August 13, 2024, from https://migrainetrust.org/understand-migraine/genetics-and-migraine/
7. Vidafar, P., McGlashan, E. M., et al. (2024). Greater sensitivity of the circadian system of women to bright light, but not dim‐to‐moderate light. Journal of Pineal Research, 76(2). https://doi.org/10.1111/jpi.12936
8. (n.d.). Women’s finer sense of smell may be due to more brain cells. Medical News Today. Retrieved August 13, 2024
9. Abbasi , A. M., Darvishi, E., et al. (2021). Gender differences in cognitive performance and psychophysiological responses during noise exposure and different workloads. Applied Acoustics, 189. https://doi.org/10.1016/j.apacoust.2021.108602